- Work Hours : Mon to Sat : 09:30- 18:30
Virtual Surgical Planning and Plates for Facial Trauma
- Designed by Zoriox Innovation Labs ,Marketed by Graft3D Healthcare Solutions
Overview
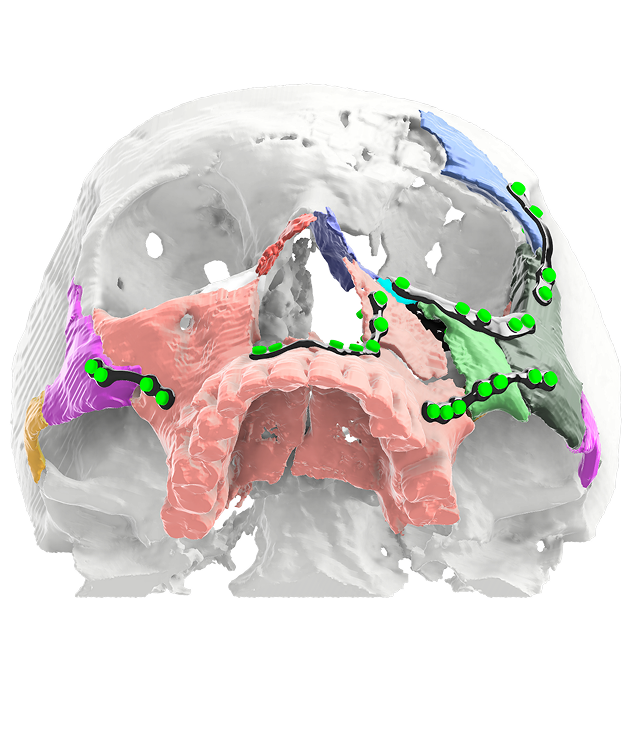
The treatment of complex facial bone fractures is challenging because of the three-dimensional anatomy of the craniofacial skeleton. The traditional methods involve intraoperative reduction and manual contouring of standard fixation plates. This extends the operation time, enhances technical challenge as well as compromises anatomical reconstruction. The adoption of Virtual Surgical Planning (VSP) and 3D printing in maxillofacial trauma care has changed the modality of patient management.
Virtual Surgical Planning in Management of Facial Trauma
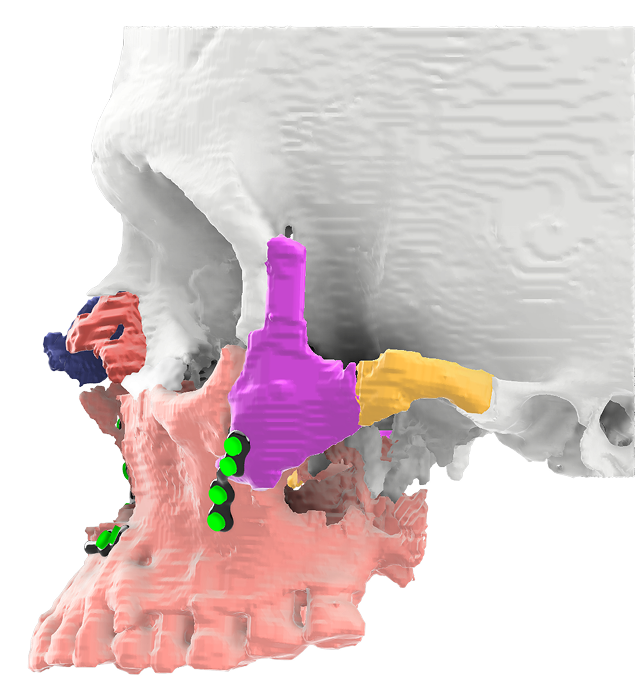
- High-resolution CT based virtual surgical planning enables the reconstruction of fractured fragments in exceptional quality.
- Surgeons are able to virtually reconstruct and manipulate bone fragments to subtitle millimeter precision, thereby producing a very accurate surgical template.
- This digitalized technique can reduce on-site guess work and increase preoperative understanding of the expected outcome.
- Patient Specific Implants such as individual titanium plates and meshes are fabricated according to the virtual planning case.
Advantages of Virtual Surgical Planning and 3D-Printed Implants
Accuracy:
- Sub-millimeter restoration of the facial anatomy.
Efficiency:
- Reduced surgical time by avoiding intraoperative plate contouring.
Predictability:
- Enhanced control through digital preoperative planning.
Improved Outcomes:
- Customized fixation plates provide long term stability, reduced complications, and better functional and aesthetic results.
Clinical Applications of Virtual Surgical Planning and 3D-Printed Implants
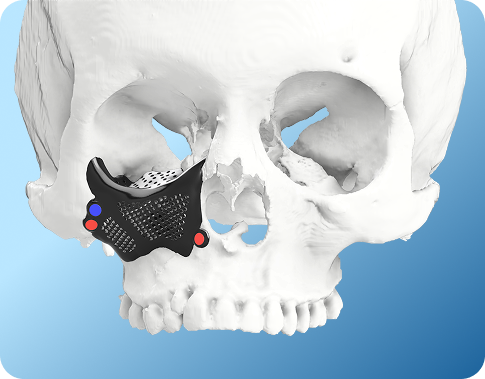
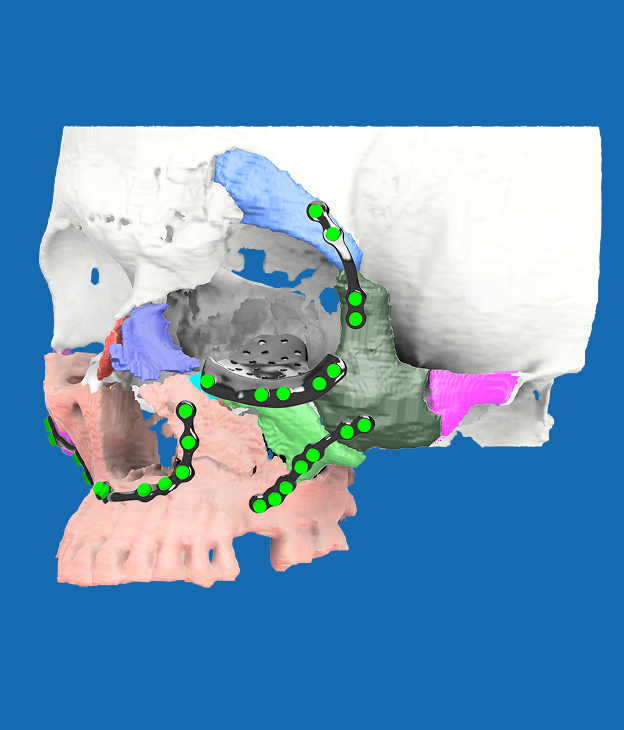
Reconstruction of the orbital fracture (Orbital wall and rim fractures):
- 3D-printed titanium plates completely reconstruct orbital structure with low risk of diplopia, enophthalmos & loss of vision.
Treatment of Zygomaticomaxillary Complex Fractures (ZMC fractures):
- Patient-specific titanium implants (PSI) restores midfacial projection, contour and symmetry. Digital preoperative planning aids in better positioning of the zygoma and maxilla than freehand techniques.
Fixation of Mandibular Fractures:
- Customized 3D printed titanium plates improve stability of the bone, occlusal alignment and jaw mobility.
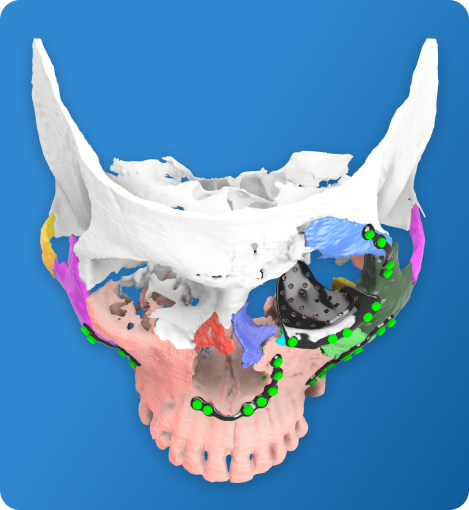
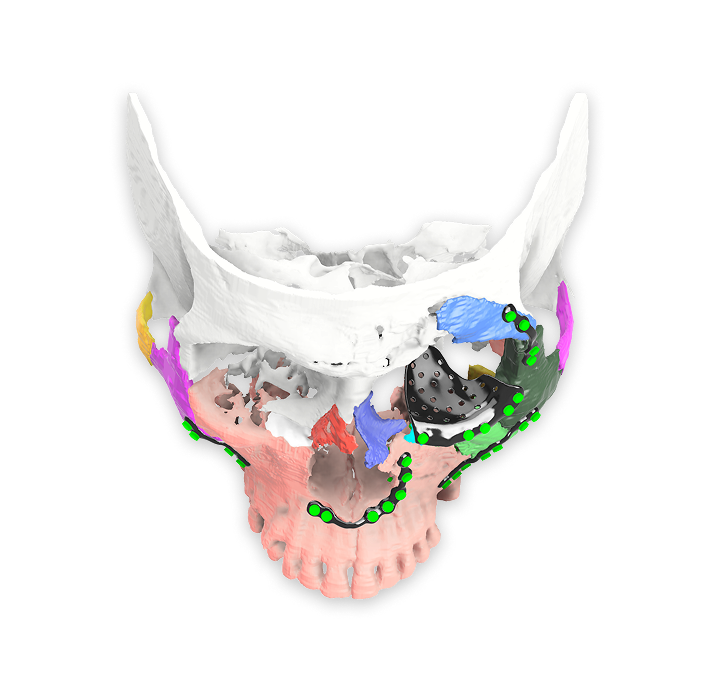
Panfacial trauma reconstruction:
- In the cases of multiple lesions,3D imaging and use of patient-specific titanium plates and meshes revises craniofacial symmetry, simplifies operation and reduces the complications.
The combination of Virtual Surgical Planning with 3D-printed titanium implants has surpassed a new standard in the treatment of facial bone reconstruction. Through integration of advanced digital imaging and surgical planning with patient-specific implants, peak accuracy, efficiency and predictability can be attained during the reconstruction of craniofacial trauma.
FAQs
What is virtual surgical planning for facial trauma?
Virtual surgical planning uses high-resolution CT data to create a 3D representation of facial fractures. This allows surgeons to plan fracture reduction, alignment, and fixation accurately before entering the operating room.
What role do 3D printed implants play in facial trauma surgery?
Virtual surgical planning with 3D printed implants allows pre-designed plates or guides to match the patient’s anatomy. This helps achieve accurate fixation, better facial symmetry, and predictable reconstruction outcomes.
When are virtual surgical planning and plates preferred over conventional methods?
They are especially beneficial in complex facial trauma cases involving multiple fractures, comminuted bone segments, or delayed reconstruction, where conventional intraoperative bending may be less accurate.
How does virtual surgical planning benefit surgeons and hospitals?
Virtual surgical planning streamlines surgical workflows by reducing operating time, minimizing intraoperative adjustments, and improving coordination between surgical teams, which is valuable for high-volume trauma centers.
Is virtual surgical planning useful for both acute and delayed facial trauma cases?
Yes, it can be applied in both acute trauma management and delayed reconstruction, helping surgeons restore facial anatomy, occlusion, and symmetry even in complex secondary cases.
Who benefits most from virtual surgical planning with 3D printed implants?
This approach benefits facial trauma surgeons seeking precision, hospitals aiming for standardized workflows, and patients who require accurate restoration of facial form and function after injury.