Virtual Surgical Planning for Mandibular Reconstruct And Design Of Resection And Cutting Guides
In recent years, there has been a significant use of CAD-CAM technology, particularly advancements in additive manufacturing (AM), for the purpose of mandibular restorations using autologous donated bone or chimeric flaps subsequent to mandibular resection. The advancement of virtual surgical planning has evolved from the initial process of planning the procedure digitally and subsequently implementing it on the patient through the use of cutting guides. This approach also involved incorporating stock plates onto anatomical models created through rapid prototyping. However, the latest development in this field involves the substitution of stock titanium reconstructive plates with patient-specific implants (PSIs) that are custom-made for each indivi The utilization of computer-assisted surgical techniques has demonstrated its reliability and efficacy in reducing surgical duration, patients’ length of hospitalisation, and overall recovery time. Additionally, these techniques have shown promising results in enhancing both functional and aesthetic outcomes. The superiority of PSIs in terms of mechanical strength has been demonstrated, resulting in a reduced risk of re-intervention for plate replacement.
The design process for mandibular reconstructive patient-specific implants (PSIs) has remained largely unaltered since its inception, with a focus on replicating the form and functionality of manually crafted stock titanium plates. The fibular or iliac crest free flaps are utilised to replace the inferior mandibular edge. These flaps are then connected to the other mandibular segments by the use of the PSI technique until the ossification of the osteotomy interfaces is fully achieved. Nevertheless, the flaps indicated earlier do not meet the necessary cross-sectional form criteria for restoring the original height of the mandible. Consequently, this results in the commonly recognised issues that arise when dental implants are implanted into bony flaps as a component of a comprehensive masticatory rehabilitation surgery.
The existing proposed interventions encompass the utilization of fibula free flap, which serves to reduce the extent of the mandibular gap that can be bridged, thereby augmenting the intricacy of the procedure. The design workflow for the reconstructive technique was established by our team, taking into account the anticipated dental rehabilitation. This involves. Our team developed a design workflow for the reconstructive procedure that already considers the removal of the defected mandible region using a resection guide (Figure 1), the adaption of fibula fragments at the defected region after defect removal (Figure 2), predicted dental rehabilitation, positioning the segments of a fibular free flap in a craniocaudal position using a fibula adaption guide (Figure 3), a fibula cutting guide (Figure 4) and a patient-specific implant (Figure 5). The utilization of conventional dental implants may be feasible, hence potentially mitigating issues associated with improper biomechanical stresses. Subsequently, the deficient vertical distance along the lower border of the mandible is addressed by employing a specially tailored component of the patient-specific implant (PSI), which serves to maintain the predetermined alignment of the fibular segments.
The DICOM data acquired from CT scans of patients’ head and neck, along with CT angiography of the legs, underwent processing using the were processed in D2P software, and Geomagic Freeform-Plus software applications. These software programmes, developed by MaterLeuven in Belgium and 3D Systems in Hill, SC, USA, were utilised to generate a virtual three-dimensional (3D) model of the patient’s facial anatomy. This model was employed to strategically plan the placement of the bony segments of the fibular free graft. The utilization of virtual dental casts was employed to facilitate the precise positioning of dental implants, taking into account the anticipated dental prosthesis.
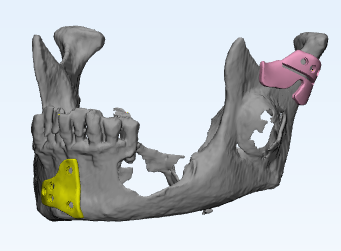
Figure 1. Mandible defect resection guides
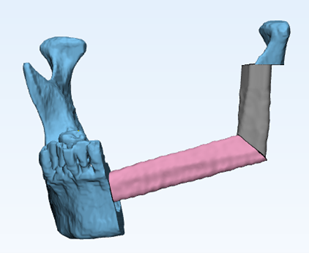
Figure 2. Fibula fragments adapted on the removed defected region of the mandible
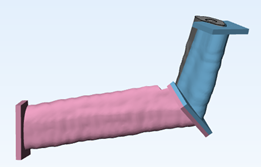
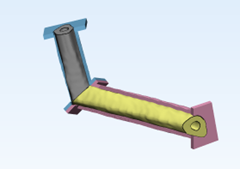
Figure 3. Fibula fragments adapted using adaptation guide
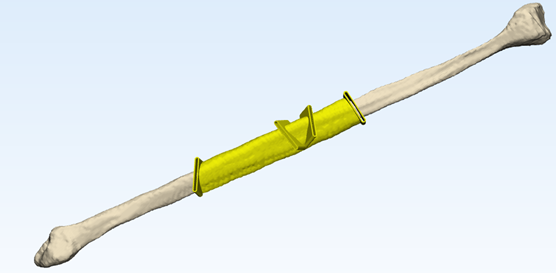
Figure 4. Fibula cutting Guide
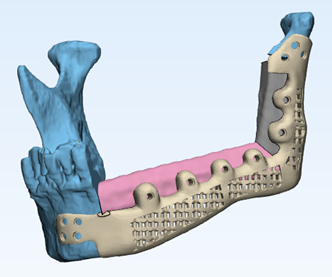
Figure 5. Patient-specific implant (PSI) with accommodation of the fibula fragments including the attachment at the condyle and the midbody of the healthy side
